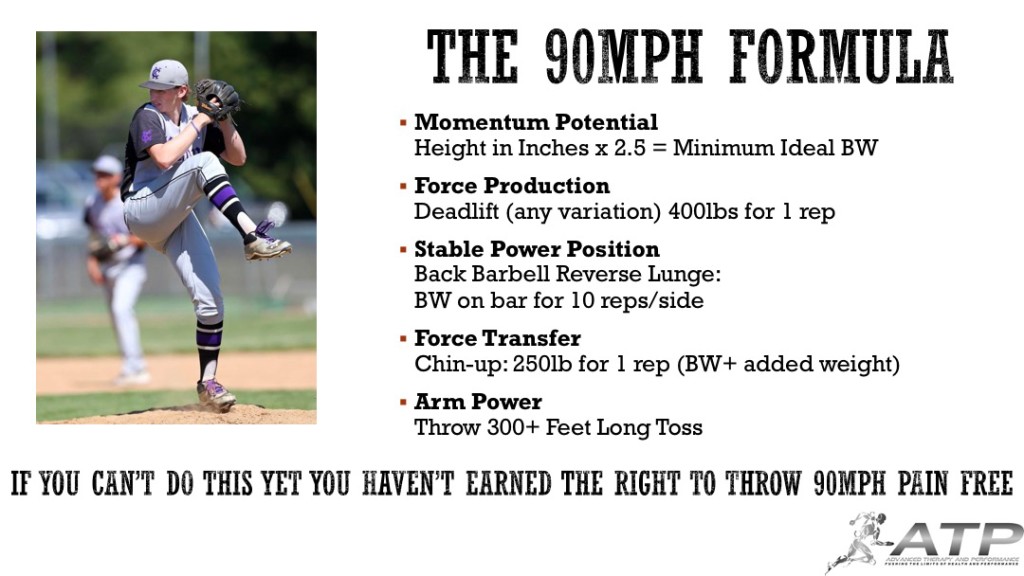
Jack Weinberger Used The 90 MPH Formula To Help Recover From Surgery & Add 12 MPH In Two Months
Jack Weinberger, free content user. I thoroughly enjoy case studies like this that highlight less than optimal training environments yet still finding a way to put in the work. I give the 90 mph formula away for free to help those willing to help themselves. The only hurdle you have is actually putting in the work and sticking to the system. Jack was able to train his lunge by using two 40 lb dumbbells and doing sets of AMRAPs. He said that the biggest factor in his weight gain was learning how to cook big healthy meals. Great work Jack!
Jack says, “The 90 mph formula and Robby Row have been incredible resources as I re-explore my mechanics post hip surgery. I feel like every time I hit a roadblock in my training, the answer was always posted the next day. Thank you!”
March 2020 #90mphformula Metrics:
Height: 6’5
Weight: 205 lbs
Height/weight coefficient: 2.66
Deadlift: 405 lbs x 1
Chin Up: 5
Reverse Lunge: 185 lbs x 1
Long Toss: 250 feet
Pull down Velocity: 84 mph
May 2020 #90mphformula Metrics:
Height: 6’5
Weight: 220 lbs
Height/weight coefficient: 2.85
Deadlift: N/A
Chin Up: N/A
Reverse lunge: N/A
Long Toss: 300 feet
Pull down velocity: 96 mph
To learn more about our remote programming services, visit our website by clicking here.
How To Stop UCL Injuries: The 90MPH Formula
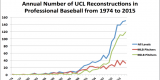
Those familiar with my work know I believe we can stop much of the UCL epidemic with proper screening, training, and logical progressions for athletes.

Camp, C. L., Conte, S., D’Angelo, J., & Fealy, S. (2017). Epidemiology of Ulnar Collateral Ligament Reconstruction in Major and Minor League Baseball Pitchers: Comprehensive Report on 1,313 Cases. Orthopaedic Journal of Sports Medicine, 5(7 suppl6).
Looking at the current research on valgus stress levels that the ulnar collateral ligament is up to 3 times weaker than the amount of force is exerted on a throw with a baseball.
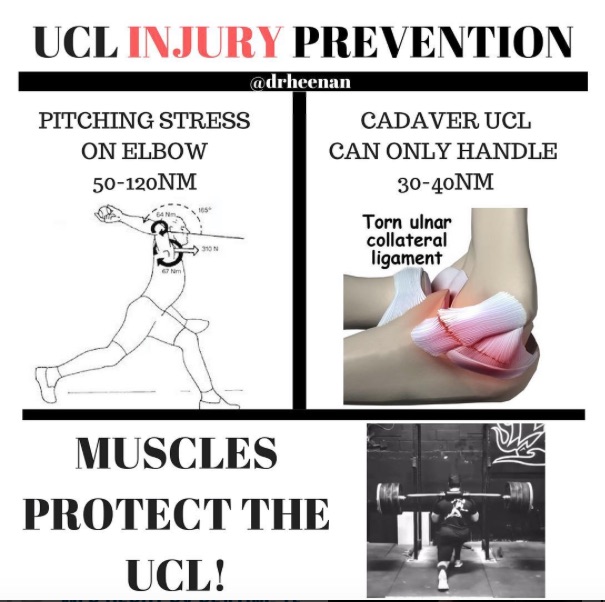
Based on our current understanding that a UCL cannot alone handle the force that throwing a baseball puts on it, we can make the case for muscular size and strength (within the specificity of the throwing motion) as main factors that protect the UCL from being strained or torn.
With 1100 baseball players having tested the criteria of the 90MPH Formula and only having 2 reported cases where an athlete could hit the metrics of the formula and needed UCL reconstruction (worth noting neither of these were our athletes local or remote clients). We have had close to 50 as of this post that reported unable to hit the parameters and had UCL reconstruction. Although the collection of the data was not done in a formalize setting, we are working on a formalized study so we can draw better correlations with quality research.
With all of these data points, we can start to draw correlations:⠀
-If you can hit the metrics, you can throw 90mph (or harder).
-If you can’t hit the metrics but can throw 90mph, you are exponentially more likely for an elbow or shoulder injury (UCL surgery most often reported).
⠀
Correlation to increased velo (in order):
1) bodyweight
2) reverse lunge
3) chin-up
4) deadlift
⠀
Correlation to decrease risk of injury (in order):
1) chin-up
2) reverse lunge
3) deadlift
4) bodyweight
⠀
My current thoughts:
-Long toss is still an underrated tool.
-Weighted balls should be used minimally prior to mastering a reverse lunge with your bw on the bar and 10 perfect bodyweight chin-ups.
-Optimal bodyweight is 2.75-3.25 x height in inches
-A 1.5x bodyweight reverse lunge is likely a replacement for 10 reps with bodyweight on the bar.
-Position players that reverse lunge 1.75x bodyweight (1rm) can run a 6.5 or less if they incorporate hill sprints and plyos as they are reaching those levels of strength.
-PO don’t sprint enough to have those strength gains carry over to elite level speed.
-Reverse lunges seem to be HIGHLY correlated to mound velocity, exit velocity, and 10/20/40/60 yard dash times.
-People seem to think I only like reverse lunges which is untrue. There are a ton of ways to increase your reverse lunge. Use what you need to get the reverse lunge to increase.
-Squatting (esp a true box squat) offer a ton of pros to getting you stronger and more athletic, they just don’t correlate to increased velo or decreased sprint times as well as lunges.
-Most high level athletes can achieve many of these numbers with one solid year of training year round. And yes, if you are not training year round I think you are going to spin your wheels for most of your career.
-Deadlift doesn’t seem to correlate well to injury prevention, but I do see a great value for it in terms of force production and adapted muscle mass. However, a 600lb deadlift doesn’t mean you should throw 110mph.
We may not have all the answers, but these correlations should allow athletes, coaches, and parents to utilize the above information in a progressive manner to start to reduce the UCL surgery epidemic we are seeing.
YOU MUST EARN THE RIGHT TO THROW HARD AND STAY HEALTHY!
Shoulder Pain in Baseball Players
Anterior (front) shoulder pain is one of the most common complaints we get from all overhead athletes especially baseball players. This pain is often palpable at the origin of the bicep tendon. Although every case can have countless pathologies (such as labral tears, impingement, poor movement mechanics) causing the pain at the bicep tendon region, about 90% of the time we find that this pain is referred pain.
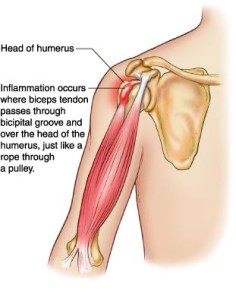
Referred pain is pain felt in a part of the body other than its actual source. Through my studies of Chinese Medicine, I can validate that many times the science and theory behind referred pain make little sense. Fortunately, pain that would be considered “bicipital tendonitis” is often very clear cut referred from the rotator cuff— most specifically the infraspinatus. The “X”s in the image below shows how the infraspinatus connects to the humerus (arm bone). Altered length, strength, movement mechanics, tissue quality or timing of the infraspinatus will throw off the mechanics of overhead movements.

To determine if this a true referred pain issue, we find the painful motion (usually reaching overhead) and have the athlete give us a number 1-10 (10 being terrible pain). After establishing a baseline for pain, we find tender points in the infraspinatus, apply firm pressure and retest the motion. This is uncomfortable for the athlete in the spot being pressed but often brings a 6-8/10 pain down to a 0-1. If that is the case, we have found the problem.
Fixing the soft tissue quality is usually done by aggressive treatment. This can be active release, cupping, Graston’s, or Gua Sha. Cupping has been the tool that gets the quickest and longest lasting results (see below). I believe this is the case because almost all therapeutic techniques are compressive in nature. Cupping offer a decompressive component often causing discoloration. Most athletes walk away pain-free in 1-2 treatments even if they have been suffering symptoms for years.
If you do not have access to a manual therapist, a lacrosse ball jammed into the infraspinatus often does the trick.
Random Thoughts – Baseball Preseason Training
With spring sports about to formally start in a few weeks, emails have been pouring in. Here is a collection of thoughts from the past week.
Training has a very profound effect on an athlete’s performance
Unfortunately, like many things in life, it takes some time to get the ball rolling and reap the full benefits of training. Do we often see outstanding results in movement, strength, and performance in a short time? Absolutely. But if you think you are going to drop .2 sec off his 60 or 40-yard dash by next week’s showcase, you are missing the point of athletic development. Skill, speed, strength, and athletic development does not happen overnight; it’s a process.
Risk can be minimized
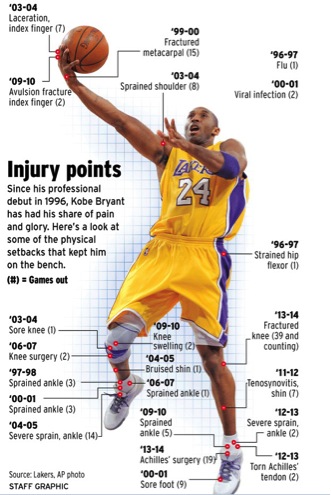
I am not a Basketball fan per se. I am however a huge fan of the qualities that a great basketball player has—hand eye coordination, great shin angles, speed, power, and endurance to name a few.
For baseball players, I can’t think of too many things with a higher risk-reward ratio than recreational/pick-up basketball. As my readers know, I am all for playing multiple sports, especially when younger, but the rate at which broken/sprained ankles, fingers, or wrists for kids “just trying to get some conditioning in” makes playing basketball not worth it unless you really love the game. With the short twenty-game New England high school baseball season, one good ankle sprain or jammed finger could mean missing half of your season.
In fact, after my 1st full season as Sacred Heart University’s Baseball Strength Coach, we forbid our players from playing basketball. Instead, I encouraged tag, dodgeball variations (not using dominant arm), and touch football.
Speed changes everything.
Rarely do you see a kid who consistently throws in the low 70s have arm pain.
Rarely do you see a kid who consistently runs an 8.0 60 yard dash pull their hamstring bad enough where they miss more than a week of their season.
Athletes and coaches need to understand how to progress throwing and speed work to mitigate short and long-term injuries. It is very difficult to have only 2-3 weeks of preseason with your team, as coaches need to make cuts and figure out whom the best players are.
Want a trick to incorporate speed and conditioning work without subjecting athletes to unneeded hamstring pulls?
Hill Sprints
Why hill sprints?
With the incline of the hill you are forcing your body into good acceleration positions, without subjecting yourself to the faster velocity required in flat ground sprints. The accelerated position also prevents over-striding and over-using the hamstrings to pull you forward (no heel landing). You want to be accelerating by pushing the ground behind you, instead of pulling you forward. So, hill sprints self corrects and teaches near optimal running mechanics without having to think about it. Hill sprints are also much more anaerobic in nature which is very applicable for baseball players. Especially the weaker, slower ones!
How do you implement this?
Week 1- Tryouts:
Start with your normal baseball skill work, but everyday at the end of practice find a steep hill and have players (pitchers included!) sprint for 20 seconds up the hill and walk back down. This can be a safe grassy hill or a pavement hill. Do 6-10 rounds of this with 2-5 minutes of recovery between sprints. Record where each player ends at the end of 20 seconds. Very quickly you will know who is “in good shape” and who is powerful and athletic. Not to mention you are avoiding god-awful distance running.
Week 2- Normal Practices:
M/W/F do 6-10 sets of 20 second hill sprints with near full recovery.
Tu/Th do 6-10 sets of 10-20 yard dashes on flat ground ~80% (full recovery in-between sets)
Week 3- Normal Practices:
M/W/F do 6-10 sets of 10-20 yard dashes on flat ground ~90% (full recovery in-between sets)
Tu/Th do 4-6 sets of 20 second hill sprints with near full recovery.
Obviously, if athletes were properly trained going into the season the coaches wouldn’t have to worry about this as much, but this is a safe way to protect the athletes and prepare them effectively.
Should You Use Ice, Aleve, or Ibuprofen After You Throw?

Ice, Aleve, or Ibuprofen plays an integral role in most pitchers’ post-outing routines. But why?
When I evaluate a new client, parents often rave about their son’s “post-game ritual” of icing right away and popping two Aleve. When I ask why they are using ice and anti-inflammatories, they always give the same answer: to stop inflammation and help recover. Yikes! There are many problems with this routine.
Problem #1 – Pain
A pitcher should not have elbow or shoulder pain post game or the day after. Muscle soreness in the upper back, rotator cuff, and deltoid is normal after an intense outing, but pain is a big no-no.
Ice, Aleve, and Ibuprofen all have analgesic or pain relieving properties. So, if a pitcher is using these modalities on a regular basis, we have no idea how their body is actually responding to throwing because the pain is masked. Being in touch with how the body feels allows us to monitor injury risks factors such as mechanical flaws, excess volume in sport or training volume, and potential sickness that may be exacerbated by lack of recovery.
Problem #2 – Delayed Recovery
Every musculoskeletal injury goes through 3 stages of recovery:
-
Inflammation
-
Repair
-
Remodeling
The following video by Kelly Starrett discusses how reducing inflammation is the wrong approach for recovery. If pressed for time start watching at 4 minutes. Don’t get bogged down by the sciency nature of the information. This is a must watch for athletes, coaches, and parents.
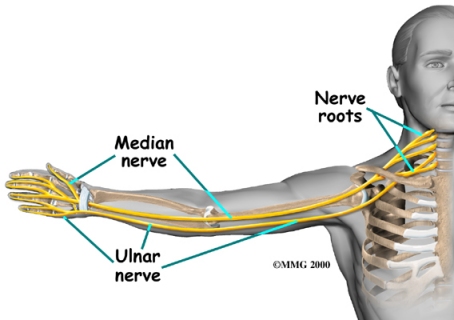
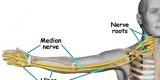
Problem #3 – Ulnar Nerve
The Ulnar Nerve is often the source of pain for athletes and non-athletes alike. Much of this can be attributed to neck pathologies and poor posture, but one thing is for sure, if you throw ice directly on the elbow about half the athletes will say it makes them feel better and the other half say it’s the most painful thing they have ever experienced.
Ulnar Nerve Transposition surgeries are common when conservative treatments no longer work and the patient experiences continual radiating pain, or pins needles with hand weakness. This portion of the elbow can be very finicky and painful, thus why I see no need to place ice directly on the elbow post throwing.
Problem #4 – Gut Health and Ulcers
Gut bacteria play an essential role in a normal digestive tract. NSAIDS can damage the mucous coating that protects the lining of the stomach. Once these bacteria damage the stomach lining, powerful stomach acid may irritate or destroy portions of the stomach. This is where ulcers often form.
Stomach ulcers can lead to excessive gas, bloating, pain or more sever issues of bleeding ulcers and cancer.
So, some changes need to be made in the common post-game routine of pitchers. Instead of settling for the conventional use of Ice, Ibuprofen, or Aleve, pitchers should follow these steps to improve recovery time and arm health:
A New Post Throwing Routine
-
Restorative Movement/Increased Blood Flow Right After Outing-
Full Body Active Warm-up -
Restorative Nutrition-
PN Injury Guide -
Restorative Sleep-
7-10 Hours of Deep Sleep -
Restorative Movement/Increased Blood Flow Next Morning-
Full Body Active Warm-up
This model of recovery is what I recommend to our pitchers and athletes who feel they need to improve their recovery techniques post game.
Notes:
-Ice and NSAIDS are not inherently bad. Instead, their application is often incorrect, as they have more applicability in a post surgical setting.
-Pain and/or swelling after throwing is not normal and should be a huge red flag that something is not right. When pain or swelling is evident seek a medical professional to evaluate the issue. Common causes are overuse, poor pitching mechanics, or orthopedic/movement/strength limitations at the ankle, hip, spine, shoulder, or elbow.
Want to take the guess work out of your in-season and off-season programming?
Check out my customized year long training program Building the Perfect Pitcher.
Move Fast, Throw Hard, Live Well – Mound Height, Throwing Programs, Links Between Foot Function and Upper Extremity Surgery
This article was shared with me by one of our in house PTs whom treats a ton of throwing shoulders. The foot starts the chain reaction of throwing. Without effective transfer of force from the foot there are links to upper body dysfunction, and in this case, surgical repair.
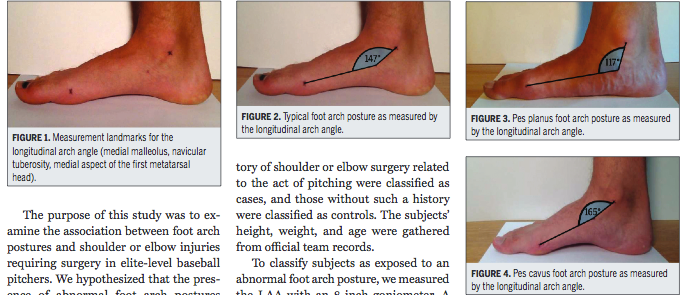
Picking out quality shoes and cleats can have a dramatic impact on ones movement and performance, make sure to get fitted by a qualified professional whom understands how your foot functions.
Pitching Mound Height Affects Throwing Motion, Injury Risk
As we head towards the pre-season, pitchers often rush themselves back to the mound in hopes to catch up to their more conditioned counterparts. Unfortunately, poor preparation and progression leave their shoulders and elbows in pain. This article gives good info on how the stress of throwing on a mound is higher than flat ground throwing. When returning to the mound, progressing methodically with a throwing program is a necessity if you want long-term health and performance.
Hip Arthroscopic and Incidences of Total Hip Replacement
Earlier today I had a video consult with a 28 year old powerlifter with femoroacetabular impingement copmaining of hip pain while squatting, and atrophy of the glute medius region. This athlete had consulted with numerous surgeons and rehab specialists trying to figure out how to address his impingement with and without surgery. As the athlete noted, some surgeons he spoke with had a good grasp of what his options were and possible outcomes, while some had no idea and offered completely outdated information.
I sent him the following literature to highlight some of the more current research on possibly dodging a total hip replacement. As stated, there are no guarantees and every case is different, but some of the facts are very much in his favor.
“Attached is research on patients whom have an arthritic hip and had arthroscopic surgery. The study tracks incidents of total hip arthroplasty post-arthroscopic debridement. Out of 564 patients in the sample, only 16% (90 patients) eventually required THA over the 7-year period. The mean age for the subjects was 55 years old.
To me, this gives high hopes for a younger athlete like yourself whom wants to avoid having total hip replacement and wishes to compete at a high level. I think the most enlightening information from this study was “75% of the patients with severe OA did not require THA by the end of the study.”1
Obviously there are lots of variables for each patient, but with a great surgeon and rehab specialist you should mitigate a ton of your long term risks.”
The incidence of total hip arthroplasty after hip arthroscopy in osteoarthritic patients
1. Haviv B, O’Donnell J. The incidence of total hip arthroplasty after hip arthroscopy in osteoarthritic patients. Sports Med Arthrosc Rehabil Ther Technol SMARTT. 2010;2:18. doi:10.1186/1758-2555-2-18.
Quinnipiac Men’s Hockey and In-Season Training

As the collegiate hockey season ends, I am sure many local Connecticut hockey players have taken special notice of Quinnipiac’s hockey present on the national level. Unfortunately, they fell just short of the national championship; nonetheless, they should be a contender in the coming years on the same stage.
For those who have had a chance to see the changes QU has made to their hockey facilities over the past ten years, its obvious that the school wanted to develop a national level program from the ground up. What many do not get to see is the countless hours of off the ice training that this team has put in.
Since 2008, Brijesh Patel has run the strength and conditioning for both men/women’s basketball and hockey programs. B is not only preparing his athletes for their current endeavors, but also building them to excel at the highest level of sport.
One aspect of training that seems misunderstood by many sport coaches is in-season training. Here B highlights some of his in season with his men’s hockey team. Coaches often look for their athletes to bust their butt in the off-season to build foundational strength and be ready for the on-field/ice rigors, but maintaining those power/strength/flexibility/mobility qualities takes hard work in-season.
My first goal as a strength and conditioning coach is to have my athletes healthy and be able to take the field. My second goal is to increase performance on the field. This means understanding how each training session plays a role in that week, month, and years cycle of development for each player. Yes, training can leave you tired, sore, and mentally drained, but a good strength coach will know how to adjust variables to not leave them feeling or preforming poorly. This is evident with a 2-month block where QU hockey didn’t lose a game.
Here at Moore in Southport, we aim for our athletes train in-season 1-3 times a week depending on their practice and game schedule. Saturday we had 70% of our baseball clientele in training from youth, high school, to pro. Each athlete has their own in-season program that is geared to keep them powerful, strong, and healthy. Many of our athletes set personal records while their in-season due to hitting growth spurts and having just the right amount of stimulus to perform at their best.
Solving Volleyball Knee Pain
Competitive volleyball is a sport plagued with countless injuries. One of the most common injuries reported is jumper’s knee.
Jumper’s knee, patellar tendonitis or patellar femoral syndrome (PFS) are the common diagnosis for “general” front of the knee, pain. Knee pain in a jumping sport can be incredibly debilitating as in many cases it can take as long as months to fully recover.
When looking at patellar tendonitis for our athletes; the first area of concern is the ankle. Acute ankle injuries make up a majority of volleyball injuries(Bahr & Bahr, 1997). Injured ankles often lack the proper mobility, mainly in dorsiflexion (e.g. limited motion foot towards the shin). As you can see in the images below, poor ankle mobility can lead to poor landing mechanics and put more stress to the knee and can irritate any existing knee pathologies or create new ones.

ACL Drop Test- also a good test for patients with knee pain.
After clearing the ankle, we usually attack hip mobility and glute strength. Any tightness in the hip flexors are going to limit the strength of our glutes, which often leads to poor movement at the knees and limited jumping power, both major qualities needed for successful volleyball play. A basic strengthening and test exercise for glute strength is a single leg bridge. We look for knees, hips and shoulders to be in one straight line.
Addressing soft tissue of the quads and glutes through foam rolling and manual therapy expedite the recovery time. Often with aggressive treatment we can see jumping athletes back on the court the same week.
Assessing overall movement followed by breaking down each joints function helps us paint a picture of why the knee is the culprit in pain; as it is usually not the dysfunctional area driving the pain.
Related Articles:
Ankle Instability: Rest vs. Early Mobilization by Craig Leibenson
Hamstring Dominance by Brijesh Patel
References
Bahr, R., & Bahr, I. A. (1997). Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scandinavian Journal of Medicine & Science in Sports, 7(3), 166–171. doi:10.1111/j.1600-0838.1997.tb00134.x
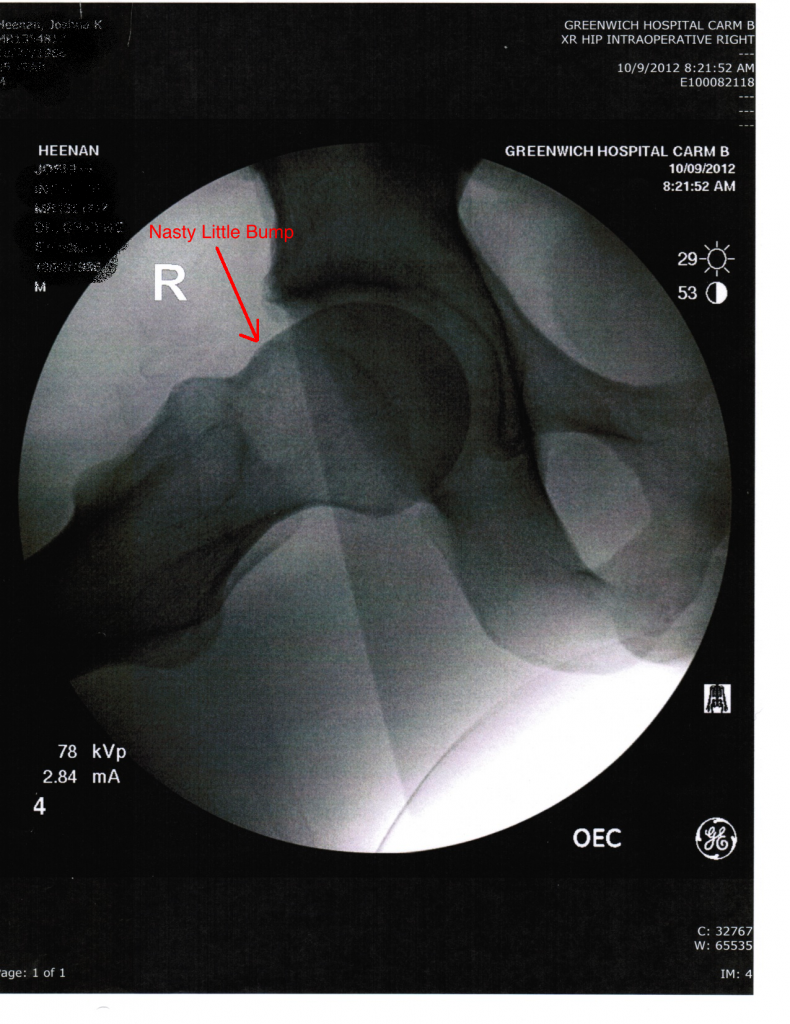
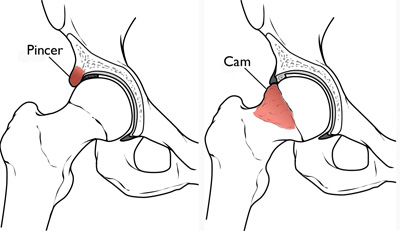
The Chronology of My Femoroacetabular Impingement (FAI) and Surgery
As I stated in my last post I recently had FAI surgery. For those who do not know exactly what FAI is, the video below does a great job of explaining the etiology and diagnosis of this condition.
Obviously, my surgery is going to be slightly different from the next persons due to the causes and restrictions of the ailment, so take everything with a grain of salt and ask questions below to allow me to clarify.
Timeline
October 2008: Did a lateral lunge while training and felt a pop in my right hip, the pain was partially in my right groin and right lower abdomen. Got checked out by a PT and we determined it to be a sports hernia. After 3 weeks of rehab, I felt good enough to resume powerlifting.
January 2009: Competed in a powerlifting meet.
February 2009-December 2009: Trained 3-5 days a week mainly for athletics and to keep my hip from hating me. PT 3x a week for 2 months followed by a month of Chiropractic work.
January 2011: Hip pain reared it’s head while deadlifting. This time it’s migrated into lower back pain (mild at worst). groin pain, and anterior hip pain.
January 2011- March 2011: Continued modified training and treatment 1-2x a week by Chiropractor, mainly on adductors.
March 2011: Went for opinion from an orthopedist on hip pain and constant “tight groin” feeling. MRI reveled some laberal damage and he wouldn’t recommend surgery.
May 2011: Second opinion from another orthopedist. New x-rays showed FAI both cam and pincer. MD suggested more PT and Chiro work.
September 2011: My right glute has highly noticeable atrophy of my glute max and what seems to be a missing glute medius. Pain is 6-8 out of 10 everyday, training brings me to an 8 consistently.
October 2011: Third opinion by one of the best hip docs in New England. In a matter of 3 minutes shows me “extreme wear, nasty laberal damage, and a nasty bump on my femoral head that is destroying my acetabulum”. He recommends getting FAI surgery once I feel I have exhausted all conservative avenues. He also warns me of the risk of a total hip replacement by the age of 40 if in the cartilage and labrum of the sock are destroyed. In the mean time I will get a cortisone shot to minimize the pain.
November 2011- May 2012: Training severely modified, work with a few new PTs whom get some relief, but overall the same.
June 2012-September 2012: Training is painful on my right lower body. I proceed to train only my left leg and upper body. Sleeping has become incredibly difficult. I am currently getting 2-4 hours of sleep almost every night and wake up feeling like I have an arthritic hip. My right glutes are no-where to be found, and I have a mild limp.
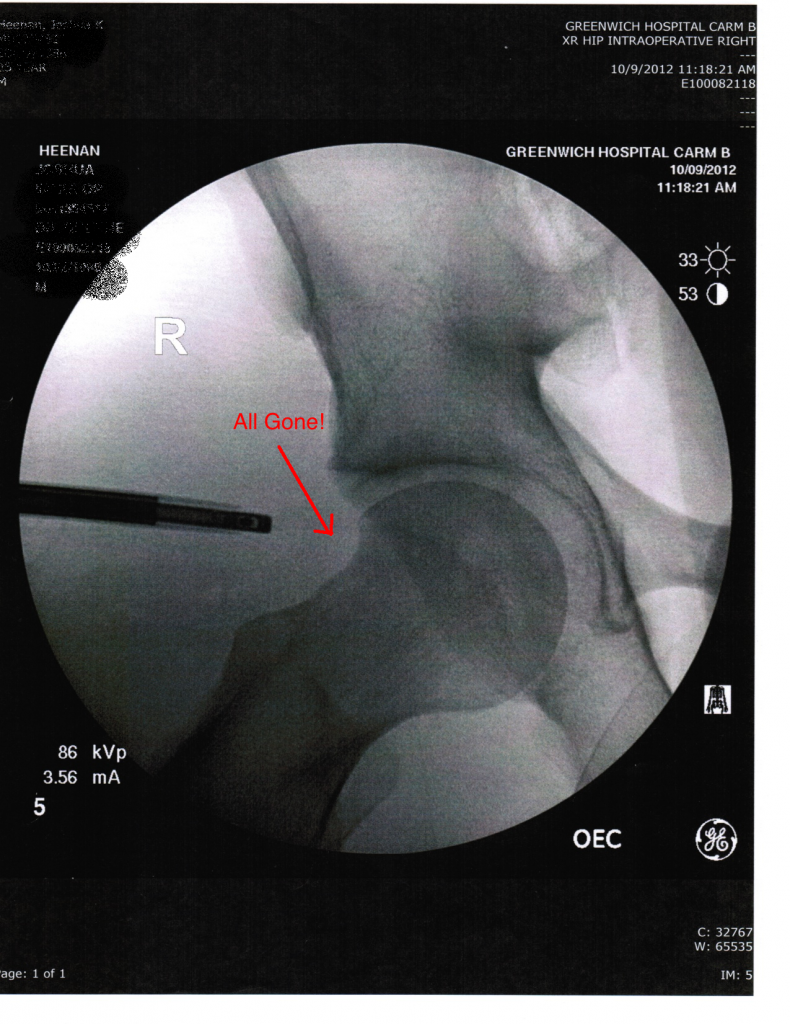
October 2012: Right FAI Surgery
3 hours of surgery
– Acetabulum is shaved down to allow more room for the femur
– Femur is shaved down to interact properly without smashing against the acetabulum, including that nasty bump that’s causing me lots of trouble.
– The labrum of my acetabulum has bone ossified in it. That area is debrided of bone and 4 sutures are put in place to repair the labrum.
– No cartilage damage was found, which was the big worry for myself and the doctor.
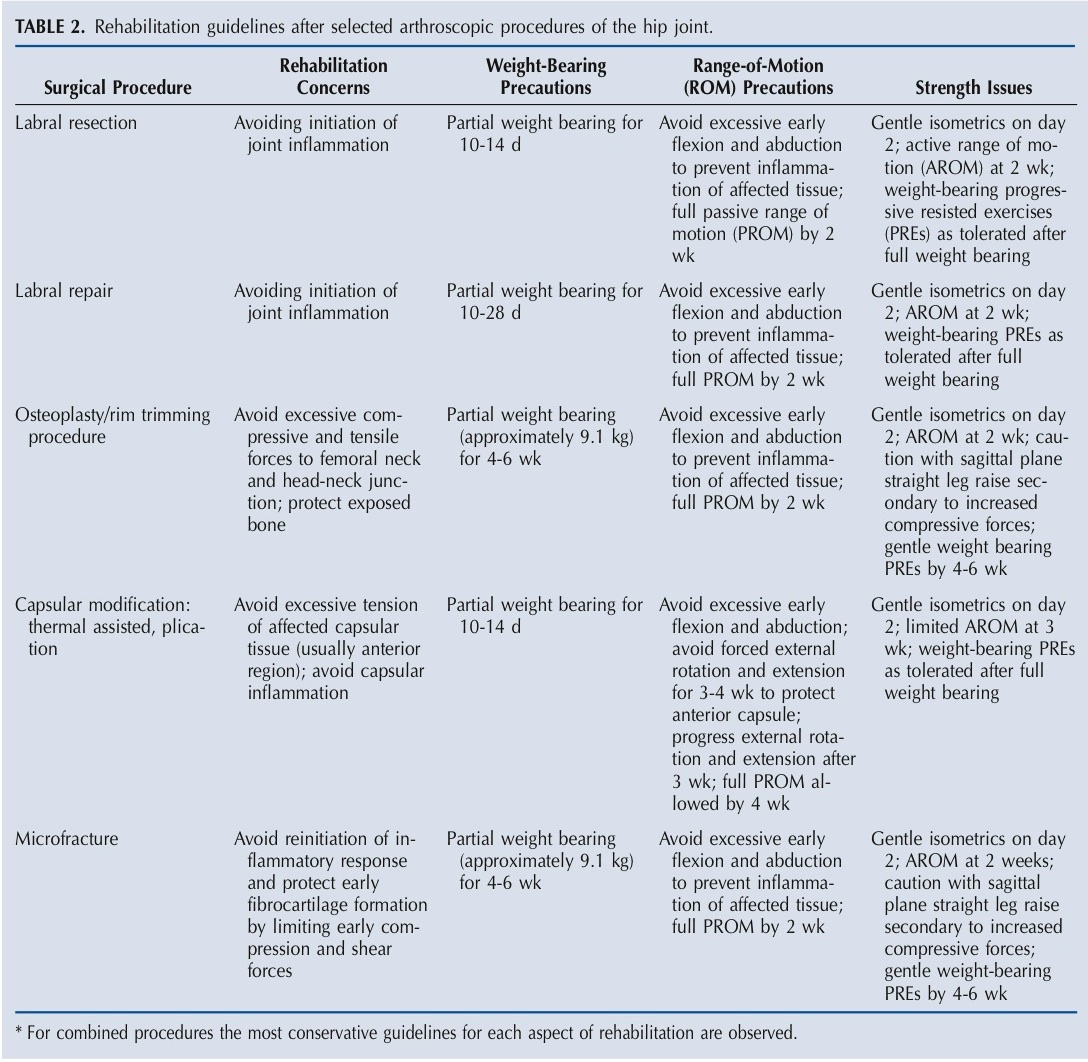
To show the variability of this procedure and the recovery; I have attached a chart of common arthroscopic procedures. Had I had cartilage damage, microfracture to the acetabulum would have been necessary and completely changed my recovery.
Currently, I am about a week out of surgery and have slept 6-9 hours a day and wake up relatively pain free.

The only thing I want to have in common with this guy is our surgeon.
Having surgery was not even a consideration 3 years ago, but pain, lack of sleep, and poor quality of life for a young active athlete was more than enough to put me over the edge. As with anything, finding the right practitioners or doctors was imperative. I believe the other doctors were timid because the average surgeon does not do many FAI surgeries and the outcomes can be very poor.
I am a long way from being back to where I was in January 2009, but having quality sleep back in my life has been an amazing change. I will continue to update my progress, feel free to comment below.
Extra Info: Here are a few great articles on FAI and how to train around it.
Femoroacetabular Impingement – Etiology, Diagnosis, and Treatment of FAI
Hip Pain in Athletes: The Origin of Femoroacetabular Impingement?
Training Around Femoroacetabular Impingement
Groin Pain – Referrals and Soft Tissue Therapy